When working in fluoroscopy, staff are regularly exposed to radiation. Therefore it is crucial for individuals to understand how to minimize one's exposure by simply being aware of the way radiation travels through their environment and positioning themselves accordingly.
Considering the complexity of these work environments, the question “What is actually out of the way?” arised quickly. We use a variety of protective equipment, but if we understand how radiation travels through a room, we can minimize our exposure by positioning ourselves effectively. So, let's put our protective gear on hold for now and focus on standing in the right place to minimize exposure.
So where should one stand in relation to the X-ray tube? In fluoroscopy, radiation exposure comes from three sources; the primary beam, the leakage of the tube, and scattered radiation. The main source of radiation for staff actually comes from the scatter of patients, rather than the tube itself. However, the position of the tube still indicates where most radiation occurs. Research [1] has shown that scattered radiation from the patient's body is more intense at the entrance side of the beam making the side opposite the beam superior for positioning oneself. Furthermore only 1 - 5% of the radiation from the direct beam reaches through the patient and less than 1% reaches all the way to the detector. Therefore, by positioning oneself on the beam exiting side of the patient one would only be exposed to patient scatter of 1-5% of the direct beam. [2]
The other most impacting factor is the distance to the X-ray source. Since radiation intensity follows the inverse square law and declines rapidly with distance (doubling distance leads to a quarter of radiation intensity). [3] Considering the work environment, unfortunately this can only be taken into consideration to a limited extent as the staff still needs to be able to operate.
So where would be the best place to stand as an operator? Ideally one would be opposite the side of the patient where the beam enters and as far away as practically possible. The worst position on the other hand would be accordingly on the side of the beam entry and as close as possible to the patient or even the direct beam.
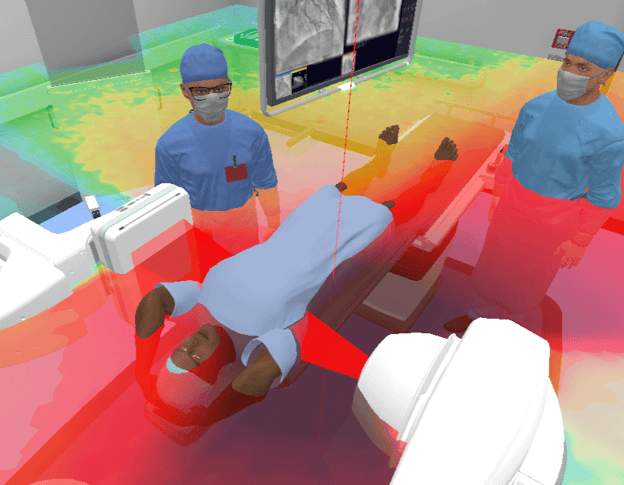
Knowing that it is impossible to completely avoid exposure when working in these environments we need to make ourselves aware of how we can manage risks for our staff. Education is crucial for any practicing staff to be able to minimize their own exposure beyond the availability of equipment and radiation protection measurements. Researchers at University College Dublin found that VR radiation dosimetry software developed by Virtual Medical Coaching was well received by medical and radiography students. Around 80% of the students enjoyed the experience, and nearly 75% reported an increase in their confidence [4]. The software, developed by Virtual Medical Coaching, creates a virtual interventional radiology suite with various equipment, surgeons, nurses, and a patient undergoing a procedure. Users can select different procedure options, such as neuro, abdominal, or cardiovascular, and observe real-time visualizations of radiation distribution and its effects on staff. This self-directed learning approach enhances curricula content and provides a valuable pedagogical tool for students to learn about radiation protection in interventional radiology.
In summary, VR radiation safety simulation offers students a practical and engaging way to learn about ionizing radiation in an intuitive and easy-to-understand manner. The immersive nature of the software, combined with real-time visualizations, allows students to experiment with different scenarios, observe the effects of radiation exposure, and develop a better understanding of radiation safety measures.
Sources :
[1] https://www.ncbi.nlm.nih.gov/books/NBK570567/
[2] https://www.ncbi.nlm.nih.gov/books/NBK564332/
[3] https://openoregon.pressbooks.pub/radsafety130/chapter/inverse-square-law/
[4] https://www.radiographyonline.com/article/S1078-8174(23)00115-3/fulltext